How we are enabling effective prevention and detection of infections within our live-in care service.
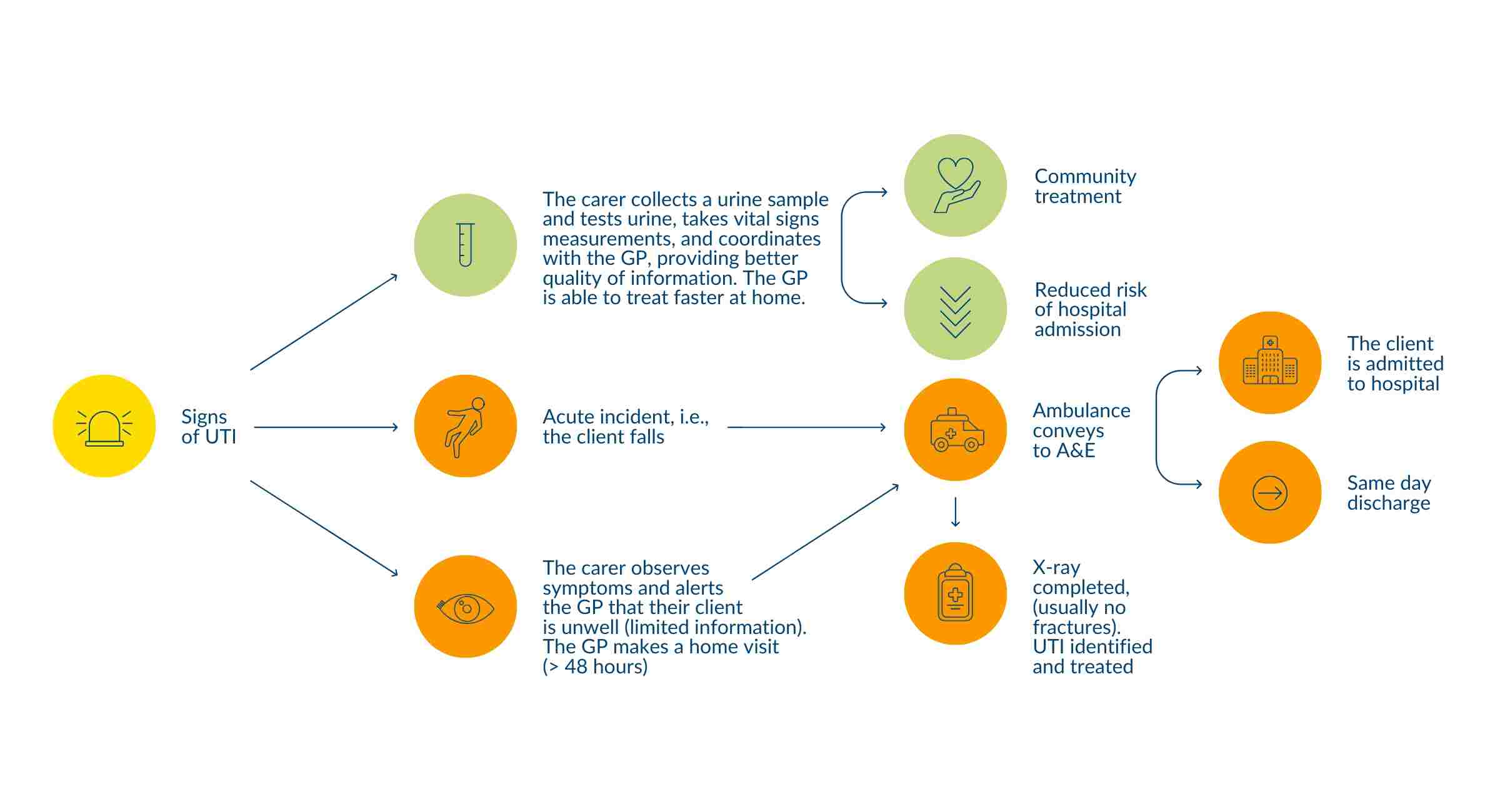
Image 1 illustrates the different trajectory for a client with a UTI pre and post implementation of urinalysis kits
The first key learning from the project was that urine samples obtained from catheter bags cannot be reliably tested for indicators of a UTI using the dipstick method. For The Good Care Group this meant emphasising these clients as high risk in training material in order that carers observe more closely for signs and symptoms unique to clients with indwelling catheters. The second key learning was that carers needed to be encouraged to pass on the results of a urinalysis test, irrespective of the results. It was important for us to communicate that professional carers are not assuming the role of the healthcare professional and should not attempt to interpret results. In order to ensure that the correct process is followed central support teams at head office now have a question on incident reports which they are required to fill in asking ‘has the GP been notified of urine test results?’.
The leading cause of hospital admissions for The Good Care Group clients is now chest infections, and this is an area which we have turned our attention to most recently. Similarly to our experience with UTI we have sought to find a mechanism for identifying chest infections early enough to enable treatment at home, rather than via emergency intervention. We have learnt that the presentation of chest infections in the elderly presents an added complication in that, often, by the time signs and symptoms can be observed, the person is typically very unwell. We have explored the health technology market, looking for something non-invasive, but with a strong track record of achieving successful outcomes. We launched a pilot programme with Feebris, a company providing AI powered vital signs monitoring kits earlier this year. We worked with around 20 clients over a period of 3 months, capturing vital sign readings using medical-grade sensors (including: temperature, blood pressure, heart rate, oxygen saturations) for early warning signs of acute respiratory illness. The measurements captured by the carer in the client’s home are reviewed by powerful AI algorithms to ensure quality and highlight abnormalities; the data can be passed onto a doctor to inform appropriate triage and accelerate access to diagnosis and treatment. The Feebris technology learns what is ‘normal’ for each individual to deliver a more personalised and holistic evaluation of people with long term conditions. We are currently in the process of completing the pilot evaluation which will determine the possibilities for future collaboration. We are hopeful that, like with the urinalysis kits, results will evidence that we can enable faster, more effective, treatment for chest infections at home with the passing on of better quality information.
The article was written by Emma Sadler, Head of Quality Assurance at The Good Care Group, and was originally published in the Journal of Dementia Care May/June 2020 issue.
The Journal of Dementia is a multidisciplinary journal for all professional staff working with people with dementia, in hospitals, nursing and residential care homes, day units and the community. The journal is committed to improving the quality of care provided for people with dementia, by keeping readers abreast of news and views, research, developments, practice and training issues. The Journal of Dementia Care is grounded firmly in practice and provides a lively forum for ideas and opinions. Full subscription information can be obtained by email at subscriptions@investorpublishing.co.uk or call 020 7104 2000.
If you’d like to find out more about The Good Care Group’s live-in care services, please contact our friendly team.
The Good Care Group is an award-winning provider of 1:1 live-in care services for the elderly. 59% of our clients are living with a form of dementia as well as a range of other conditions. For the individuals that we support an infection can have a wide-reaching impact on health and well-being.
As part of our overall commitment to quality we regularly review our client incident data and in early 2017 began to see that urinary tract infections (UTI) were the number one reason our clients were admitted to hospital, as well as being the cause of many falls, incidents of distressed behaviour and periods of being generally unwell. For our clients who wish to receive care in the comfort of their own home hospital is one of the worse places they can be. It is widely recognised that people with dementia do not fare well in acute hospital settings; they can be confusing, distressing places, and often elderly people, especially those with dementia, do not bounce back to their original state of health following a stay. It is for this reason that we have worked hard over the past 2 years to reduce incidents of infections, focussing first on UTI and more recently, chest infections.
Our Quality Assurance team recognised, through analysis, that live-in carers are uniquely placed to identify signs and symptoms of a UTI but that there was an opportunity to improve the quality of information that they were passing on to healthcare professionals. For example, an all too common narrative was that a professional carer would report to the client’s Doctor their observation of the client being ‘out of sorts’, a GP would take this information and advise the carer to monitor the client. Later in the day (often out of hours) the client would become acutely unwell, the carer would telephone 111 and communicate their concerns to an out of hours Doctor unfamiliar with the client which would result in a trip to A&E or a hospital admission. Looking to find a way to empower professional carers to be able to narrow down the issue the client was experiencing we chose to introduce urinalysis testing kits to each of our client placements with enhanced training for professional carers. Urinalysis kits enable a professional carer to dipstick a client’s urine sample and capture information about potential abnormalities. Whilst carers are not diagnosing urinary tract infections they are able to pass on a better quality of information. It avoids the scenario described above and instead means that professional carers are able to give the client’s GP information about not only the symptoms they have observed but also the levels of various substances such as protein and ketones present within the urine. We have typically found that healthcare professionals are able to respond quicker to this type of information, enabling swift treatment for clients at home.
The kits are low cost and easy to obtain. An important feature of the planning process was to ensure that the training strategy we devised suited the needs of a remote and spread out workforce. The Good Care Group provide care for almost 400 people across England and Scotland and so kits had to be packaged up centrally and manually posted to each placement. We opted to take 6 months (May to December) to introduce the kits to one regional locality at a time. We took time to provide resources and training videos on infection prevention, signs and symptoms of UTI and use of the dipstick kits before organising distribution. We also made use of online quizzes sent out in a weekly newsletter, provided face-to-face training for existing carers and introduced a module on urinalysis to our mandatory induction training for all new staff.
The Good Care Group are incredibly proud of the successful outcomes we have been able to evidence as a result of this project. Through the introduction of urinalysis testing kits we were able to reduce emergency intervention (UTIs involving a 999 call or ambulance call out) by a staggering 63%. A 22% reduction in overall UTI related hospital admissions was also achieved. If applying a cost saving to these interventions we can say that reductions in emergency-ambulance intervention and admission rates achieved a 70% and 32% cost saving for the NHS, respectively. These results are highly significant, not only in terms of potential cost savings and efficiencies for the NHS, but also as a demonstration of what can be achieved when social care providers seek to collaborate with health care services. Most importantly, the intervention resulted in much improved health and well-being outcomes for some of the most vulnerable people in our society. Interestingly, in the 6 months following the introduction of urinalysis kits the number of UTIs diagnosed actually increased. This is likely because professional carers were better trained to spot potential signs and symptoms and infections were less likely to go undetected.
Image 1